Practice changing results for those with the BRAF V600E mutation were presented by Australian of the Year Professor Georgina Long at ASCO last month.
Twelve months of targeted drug therapy after complete lymph node dissection has significant benefit in preventing disease progression in BRAF positive Stage III melanoma patients, say researchers.
Final results of the COMBI-AD clinical trial were published last week in the New England Journal of Medicine, and presented by joint 2024 Australian of the Year Professor Georgina Long AO at last month’s American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago.
Professor Long is also co-medical director of the Melanoma Institute Australia, one of the biggest contributors of patients to the trial testing targeted therapies that block the genetic mutations which cause a cancer cell to grow and spread.
“This long term follow-up data shows significant benefit to be maintained at nearly 10 years, and is likely to be one of the only adjuvant trials in melanoma to show a difference in the overall survival with the use of adjuvant drug therapy,” she said.
“This confirms the impact of dabrafenib and trametinib as a standard therapy in resected stage III melanoma, especially for patients with the BRAF V600E mutation.”
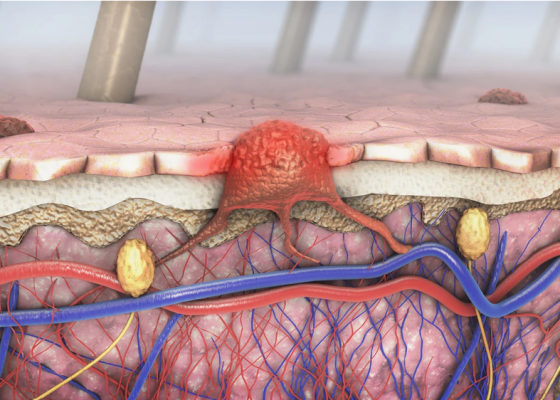
About 40% of patients with melanoma have a BRAF mutation which can be blocked by giving BRAF and MEK inhibitor drugs. These drugs have been shown to be effective for patients with advanced melanoma.
The COMBI-AD trial aimed to determine whether giving a BRAF inhibitor (dabrafenib) and MEK inhibitor (trametinib) to Stage III patients for 12 months after they had complete lymph node dissection would prevent their melanoma recurring and becoming Stage IV.
Professor Long told ASCO that in the dabrafenib plus trametinib arm, the 10-year rate for relapse-free survival was 48%, and for distant metastases-free survival was 63% (compared with 32% and 48% respectively in the placebo arms).
The first and final analysis for overall survival was also presented, and dabrafenib plus trametinib reduced the risk of death by 20%. This was reduced even more in those with the BRAF V600E mutation in their melanoma, by 25%.
Co-author and medical oncologist at Alfred Health in Melbourne, Associate Professor Andrew Haydon, told Dermatology Republic the findings will undoubtedly change practice.
“What this data gives us is an is an option to give those patients with a BRAF mutation this targeted therapy which doesn’t have any long term toxicity risk, no permanent toxicity and a survival benefit,” he said.
“So in my mind, for patients with a V600E mutation, targeted therapy is clearly the preferred adjuvant treatment over immunotherapy.
“That’s been my thought for many years, for as long as we’ve had initial results come out. But I would say that for many years I’ve been in the minority there, and most clinicians have favoured immunotherapy over targeted therapy.
“I think this might swing it back the other way.”
However Professor Haydon did point out that while there were benefits for patients with the BRAF V600E mutation, this was not the case for those with the BRAF V600K mutation.
“This is also very clear data that would suggest that if you’ve got a v600K mutation, then you would use immunotherapy in preference to targeted therapy,” he said.
“So I would stop giving the V600K patients targeted therapy, and either watch and wait, or give immunotherapy.”
Also released at ASCO and published in the NEJM were the practice-changing results of the NADINA clinical trial, which showed drug therapy before surgery to be effective in preventing disease progression in high-risk Stage III melanoma patients.
Professor Long led the Australian arm of the NADINA trial which was opened at eight centres around the country.
“Both the COMBI-AD and NADINA trials have been critical in transforming melanoma clinical care, and we are proud that Melanoma Institute Australia and our patients have played a leading role in both trials,” said Professor Long.
“To have both papers published recently in the prestigious New England Journal of Medicine shows MIA’s global impact in continuing to push science and medicine forward.”
New England Journal of Medicine 2024, online 19 June
New England Journal of Medicine 2024, online 4 June